Stem Cell Lymphocytic Leukemia: Conditions and Indications
Stem cell therapy has transformed the way many blood-related cancers are treated, especially different forms of leukemia. Among these, lymphocytic leukemia stands out as a condition where advanced medical approaches, including stem cell transplantation, can significantly improve survival and quality of life. Understanding the conditions and indications for stem cell treatment in lymphocytic leukemia helps patients and families make informed decisions about care options, treatment pathways, and long-term outcomes.
In leading medical centers like Liv Hospital, stem cell therapies are offered using internationally recognized protocols, modern diagnostic tools, and multidisciplinary care teams. These treatments are carefully selected based on the type of leukemia, the patient’s health status, and disease progression.
Understanding Lymphocytic Leukemia
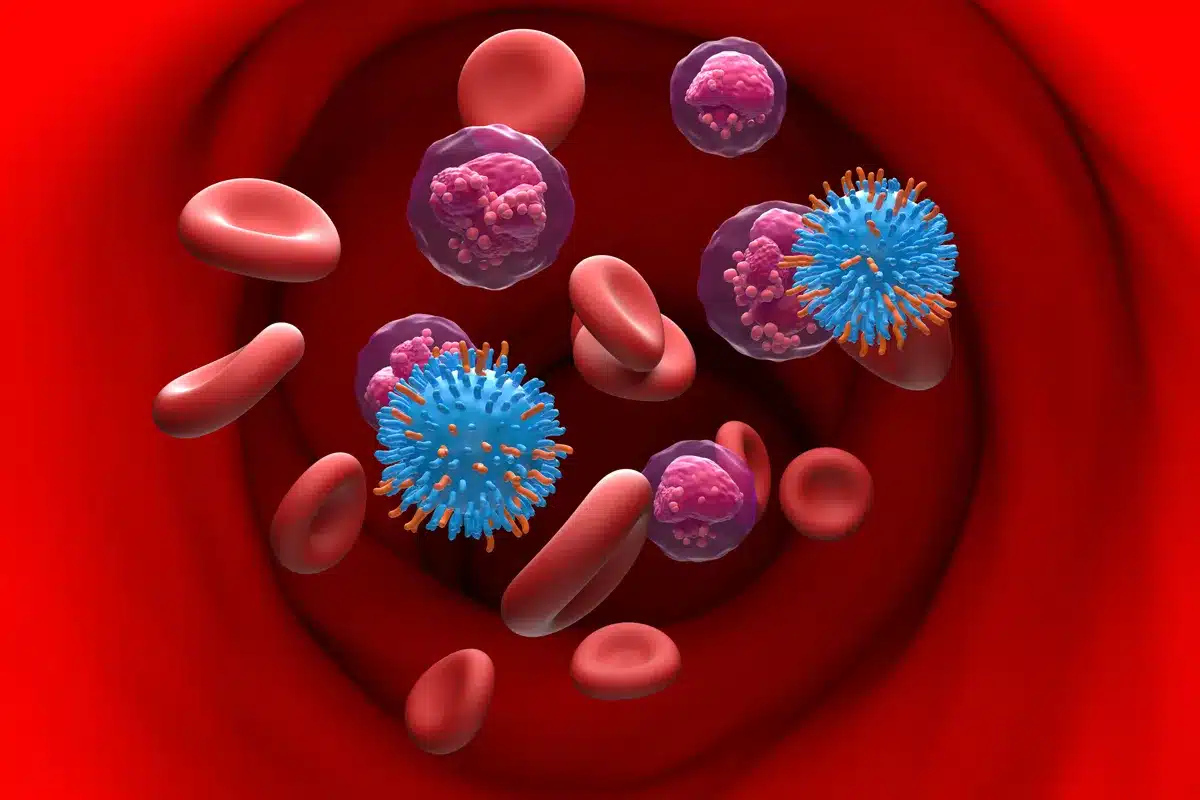
Lymphocytic leukemia is a type of blood cancer that affects lymphocytes, which are white blood cells responsible for immune defense. These abnormal cells multiply uncontrollably in the bone marrow, blood, and sometimes lymph nodes or spleen. As a result, healthy blood cell production is disrupted, leading to symptoms such as frequent infections, fatigue, anemia, bruising, and weight loss.
There are two main types:
- Acute Lymphocytic Leukemia (ALL): Rapidly progressing and more common in children.
- Chronic Lymphocytic Leukemia (CLL): Slowly progressing and more common in adults.
Both types may require stem cell therapy in specific clinical situations.
What Is Stem Cell Therapy?
Stem cell therapy, also known as hematopoietic stem cell transplantation (HSCT), involves replacing damaged or cancerous bone marrow with healthy stem cells. These stem cells can regenerate normal blood cells and rebuild the immune system.
There are two main types of stem cell transplants:
- Autologous transplant: Uses the patient’s own stem cells.
- Allogeneic transplant: Uses stem cells from a compatible donor.
In lymphocytic leukemia, allogeneic transplants are more commonly used because they provide a new immune system that can help fight residual cancer cells.
Conditions Requiring Stem Cell Therapy
Stem cell transplantation is not recommended for every patient with lymphocytic leukemia. It is usually advised under specific conditions where standard treatments like chemotherapy or targeted therapy are not sufficient.
Some key conditions include:
1. High-Risk Leukemia
Patients with aggressive genetic mutations or poor response to chemotherapy are considered high-risk and may benefit from early stem cell transplantation.
2. Relapsed Leukemia
If leukemia returns after initial treatment, stem cell therapy is often recommended as a curative option.
3. Refractory Leukemia
When leukemia does not respond to standard therapies, stem cell transplantation may be the only effective treatment left.
4. Advanced Disease Stage
In later stages of CLL or ALL, when complications arise, stem cell therapy can offer long-term remission.
Indications for Stem Cell Transplantation
Doctors consider several clinical indicators before recommending stem cell treatment. These indications are based on medical guidelines and individual patient assessments.
Key Medical Indications
- Failure of first-line chemotherapy
- Presence of unfavorable genetic markers
- Multiple disease relapses
- Severe bone marrow failure
- Young age with aggressive disease
- Availability of a suitable donor
Each patient undergoes detailed diagnostic testing, including blood tests, bone marrow biopsy, imaging scans, and genetic profiling before final treatment decisions.
For a comprehensive medical overview, you can explore this detailed resource on Stem Cell Lymphocytic Leukemia Conditions and Indications.
Patient Eligibility for Stem Cell Therapy
Not every patient qualifies for stem cell transplantation. Eligibility depends on several personal and medical factors, such as:
- Age and overall physical condition
- Organ function (heart, liver, lungs, kidneys)
- Infection status
- Disease stage and response to treatment
- Psychological readiness and support system
Doctors carefully evaluate risks versus benefits, as stem cell therapy can involve complications like graft-versus-host disease (GVHD), infections, and immune suppression.
The Stem Cell Transplant Process
The treatment process typically includes several stages:
1. Pre-Transplant Evaluation
Comprehensive health assessment and donor matching.
2. Conditioning Therapy
High-dose chemotherapy or radiation to destroy cancerous cells and suppress the immune system.
3. Stem Cell Infusion
Healthy stem cells are infused through a vein, similar to a blood transfusion.
4. Engraftment and Recovery
Stem cells begin producing new blood cells, which may take several weeks.
5. Long-Term Monitoring
Regular follow-ups to monitor immune recovery and detect any complications.
Benefits of Stem Cell Therapy in Lymphocytic Leukemia
Stem cell transplantation offers several potential advantages:
- Long-term remission or cure
- Rebuilding of healthy immune system
- Reduced dependency on repeated chemotherapy
- Improved survival rates for high-risk patients
- Better disease control in relapsed cases
Although not risk-free, for many patients, stem cell therapy provides the best chance for long-term recovery.
Risks and Possible Complications
While stem cell therapy is highly effective, it may involve certain risks:
- Infections due to weakened immunity
- Graft-versus-host disease (GVHD)
- Organ toxicity
- Fatigue and nutritional issues
- Emotional and psychological stress
These risks are managed through strict monitoring, medications, and supportive care protocols.
Role of Specialized Hospitals in Treatment
Hospitals with dedicated stem cell units play a critical role in successful outcomes. Institutions like Liv Hospital offer:
- Advanced transplant facilities
- International donor registries
- Multidisciplinary medical teams
- Modern infection control systems
- Personalized patient care programs
Such infrastructure ensures safer procedures and improved survival outcomes.
Recovery and Quality of Life After Transplant
Recovery after stem cell transplantation varies for each patient. Some individuals return to normal life within months, while others need longer rehabilitation. Lifestyle adjustments often include:
- Balanced nutrition
- Infection prevention
- Regular medical checkups
- Mental health support
- Gradual return to daily activities
Long-term follow-up is essential to ensure sustained remission and overall well-being.
Conclusion
Stem cell therapy has become a cornerstone in the treatment of lymphocytic leukemia, especially for high-risk, relapsed, or treatment-resistant cases. By understanding the conditions and indications for transplantation, patients can make more informed choices about their care journey. With advancements in medical science and specialized treatment centers, stem cell therapy now offers hope for long-term remission and improved quality of life for many individuals facing lymphocytic leukemia.
In addition to medical treatment, overall wellness and lifestyle play an important role in recovery and long-term health. Resources like live and feel provide valuable insights into maintaining physical, emotional, and mental well-being during and after serious health conditions.
FAQs
1. What is lymphocytic leukemia?
Lymphocytic leukemia is a blood cancer that affects lymphocytes, a type of white blood cell involved in immune defense. It can be acute or chronic and disrupts normal blood cell production.
2. When is stem cell therapy recommended?
Stem cell therapy is recommended for high-risk cases, relapsed leukemia, treatment-resistant disease, or advanced stages where standard therapies fail.
3. Is stem cell transplant a cure for leukemia?
In many cases, stem cell transplantation can lead to long-term remission or cure, especially in younger patients with suitable donors and good overall health.
4. What are the risks of stem cell transplantation?
Risks include infections, graft-versus-host disease, immune suppression, and organ complications, but these are managed through advanced medical care.
5. How long does recovery take after transplant?
Recovery varies but usually takes several months. Full immune system recovery can take up to a year or longer, depending on individual health factors.
6. Can older patients undergo stem cell therapy?
Yes, but eligibility depends on overall health, organ function, and disease severity rather than age alone.